What is an anterolateral ligament (ALL) reconstruction?
In the latest ACL-reconstructions, the anterolateral ligament (ALL) is used a lot! To help understand an ALL reconstruction we wrote this blog.
Anterolateral ligament (ALL) reconstruction is, as the names says it, a reconstruction of your ALL. The ALL is a ligament located at the lateral side of the knee, between the femur and the tibia. The reconstruction helps in the stability of the knee.
Do you want to know everything about the ALL reconstruction in combination with ACL reconstruction and what the ALL does? Take some time to read this blog about everything including the ALL.
What is the anterolateral ligament (ALL)?
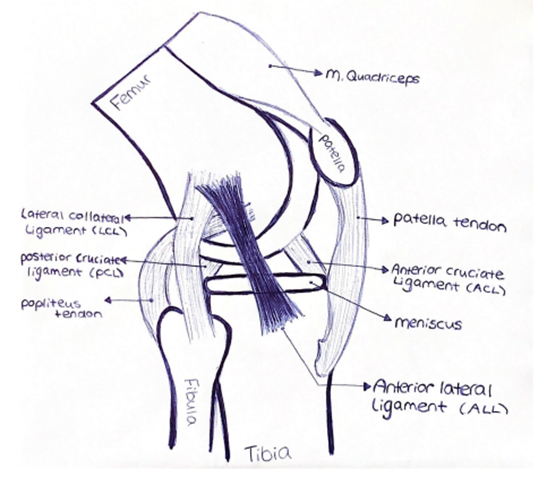
At first, there are several descriptions of the ALL. We decided to pick one study from Claes S. et al.(1) to describe what the ALL is. They found a ligamentous structure on the anterolateral side of the knee. This ligament showed a connection of the femur with the tibia.
The origin of the ALL is on the lateral femoral epicondyle, anterior to the origin of the lateral collateral ligament (LCL).
The insertion is located between the Gerdy’s tubercle and the head of the fibula. We tried to make our own illustration of the ALL in the picture above.
What is the function of the Anterolateral ligament (In combination with other ligaments, such as the anterior cruciate ligament (ACL)?
A few studies described the function of the ALL (in combination with other ligaments) and showed that it was an important ligament in the knee joint.
Firstly, it prevents passive internal rotation of the tibia.(2,3) Secondly, it prevents anterior tibial subluxation at 60° of knee flexion.(4)
In conclusion, one article states: “The results highlight the clinical relevance of this structure (ALL) that should be assessed before an ACL reconstruction in order to avoid residual laxity.”(3)
However, an article written by Jin Kyu Lee et al. said that there were inconsistent results in the resisting of internal rotation of the tibia and anterior subluxation of the tibia.(5)
How do you rupture your ALL?

The ALL often ruptures in combination with your ACL.
70% of all ACL ruptures are based on a “non-contact” trauma mechanism.(6,7) This usually occurs as a result of a sudden deceleration while changing direction, running or landing after a jump. The incidence is highest in people aged 15-40 years who play pivotal sports, such as basketball, football, handball, and/or skiing.(8,9)
In addition, ACL injuries are most common in female athletes than in male athletes, who participate in similar sports.(10,11,12)
There are a number of risk factors that affect motor control for non-contact ACL injury: greater knee valgus during landing, limited knee flexion during landing, increased vGRF during landings with relatively more extended knees and limited trunk flexion during landing.(13,14)
We have written another article about the use of an external focus in ACL rehabilitation on the risk factors we stated above.
What are the indications for ALL reconstruction?
A review from Matthew J. Kreautler et al. describes the indications of an ALL reconstruction perfectly.(15) We decided to get a few points out of this review.
The indications for ALL reconstruction were not quite clear. A lot of literature stated ALL reconstruction should be done with patients with a high-grade pivot shift (grade 2-3).
However, a few studies stated no effect of pivot shift on revision rate or postoperative instability after primary ACL reconstruction.
Personally, we mostly agreed with the following statement written in the review: “Some authors advocate for ALL reconstruction based on patient activities, such as participation in pivoting sports or in high-level or “elite” athletics, and in patients demonstrating attributed of hypermobility.”(15,16,17)
The rehabilitation after an ALL reconstruction
The rehabilitation of an ALL reconstruction is not much different than an ACL reconstruction. A patient can be kept in a brace until he or she is able to perform an unassisted straight leg raise.
We advise to use crutches for a minimum of at least 2 weeks, due to the extension needing to be back to normal. From week 2 we advise to build up your load.
After 6 till 9 months, the patient can return to sport. This is always after a consultation with a (sport)physiotherapist. Our clients will therefore always need to complete the return to sport tests above 85-90% limb symmetry index (LSI).
Sources:
- Claes, S., Vereecke, E., Maes, M., Victor, J., Verdonk, P., & Bellemans, J. (2013). Anatomy of the anterolateral ligament of the knee. Journal of Anatomy, 223(4), 321–328. doi:10.1111/joa.12087
- Ruiz, N., Filippi, G. J., Gagnière, B., Bowen, M., & Robert, H. E. (2016). The Comparative Role of the Anterior Cruciate Ligament and Anterolateral Structures in Controlling Passive Internal Rotation of the Knee: A Biomechanical Study. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 32(6), 1053–1062. doi:10.1016/j.arthro.2016.02.017
- Bonanzinga T, Signorelli C, Grassi A, Lopomo N, Bragonzoni L, Zaffagnini S, Marcacci M. Kinematics of ACL and anterolateral ligament. Part I: Combined lesion. Knee Surg Sports Traumatol Arthrosc. 2017 Apr;25(4):1055-1061. doi: 10.1007/s00167-016-4259-y. Epub 2016 Sep 8. PMID: 27631644.
- Monaco, E., Ferretti, A., Labianca, L., Maestri, B., Speranza, A., Kelly, M. J., & D’Arrigo, C. (2011). Navigated knee kinematics after cutting of the ACL and its secondary restraint. Knee Surgery, Sports Traumatology, Arthroscopy, 20(5), 870–877. doi:10.1007/s00167-011-1640-8
- Lee, J.K., Seo, Y.J., Jeong, SY. et al. Biomechanical function of the anterolateral ligament of the knee: a systematic review. Knee Surg & Relat Res 32, 6 (2020). https://doi.org/10.1186/s43019-019-0021-3
- Quatman CE, Hewett TE. The anterior cruciate ligament injury controversy: is ‘valgus collapse’ a sex-specific mechanism? Br J Sports Med. 2009;43(5):328-35.
- Saris DBF, Diercks RL, Meuffels DE, Fievez AWFM, Patt TW, Hart CP van der, et al. Richtlijn voorste kruisbandletsel Nederlandse Orthopaedische Vereniging. 2011. Available from: http://www.kwaliteitskoepel.nl/assets/structured-files/2011/voorste_kruisband.pdf.
- Prodromos CC, Han Y, Rogowski J, Joyce B, Shi K. A meta-analysis of the incidence of anterior cruciate ligament tears as a function of gender, sport, and a knee injury-reduction regimen. Arthroscopy. 2007;23(12):1320-5.
- Moses B, Orchard J, Orchard J. Systematic review: annual incidence of ACL injury and surgery in various populations. Res Sports Med. 2012;20(3-4):157-79.
- Agel J, Arendt EA, Bershadsky B. Anterior cruciate ligament injury in National Collegiate Athletic Association basketball and soccer: a 13- year review. Am J Sports Med. 2005; 33:524-531
- Messina DF, Farney WC, DeLee JC. The incidence of injury in Texas high school basketball. A prospective study among male and female athletes. Am J Sports Med. 1999; 27:294-299.
- Malinzak RA, Colby SM, Kirkendall DT, Yu B, Garrett WE. A comparison of knee joint motion patterns between men and women in selected athletic tasks. Clin Biomech (Bristol, Avon). 2001;16: 438-445.
- Castanharo R, da Luz BS, Bitar AC, D’Elia CO, Castropil W, Duarte M. Males still have limb asymmetries in multijoint movement tasks more than 2 years following anterior cruciate ligament reconstruction. J Orthop Sci. 2011;16(5):531–5
- Sigward SM, Powers CM. The influence of gender on knee kinematics, kinetics and muscle activation patterns during side-step cutting. Clin Biomech (Bristol, Avon). 2006; 21:41-48.
- Kraeutler MJ, Welton KL, Chahla J, LaPrade RF, McCarty EC. Current Concepts of the Anterolateral Ligament of the Knee: Anatomy, Biomechanics, and Reconstruction. Am J Sports Med. 2018 Apr;46(5):1235-1242. doi: 10.1177/0363546517701920. Epub 2017 Apr 20. PMID: 28426251.
- Smith JO, Yasen SK, Lord B, Wilson AJ. Combined anterolateral ligament and anatomic anterior cruciate ligament reconstruction of the knee. Knee Surg Sports Traumatol Arthrosc. 2015;23(11):3151-3156.
- Sonnery-Cottet B, Barbosa NC, Tuteja S, Daggett M, Kajetanek C, Thaunat M. Minimally invasive anterolateral ligament reconstruction in the setting of anterior cruciate ligament injury. Arthrosc Tech. 2016;5(1):e211-e215.